Western Medicine and the Health of the People of the African Diaspora
Though they belonged to a healing profession and pledged to ‘First do no harm’, physicians in the Antebellum:
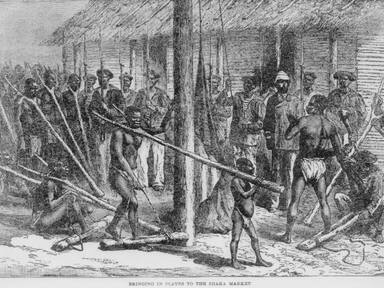
- Worked at slave markets attesting to the health of enslaved peoples to improve the profitability of the slave trade.
- performed experimental surgeries on enslaved women to develop techniques, procedures, and instruments. J. Marion Sims was the most famous because he was self-promoting, but there were several documented early Gynecologists who honed their craft on enslaved women. They also trained the women who were recovering from surgery as surgical assistants according to historian Deidre Cooper Owens.
- used no anesthesia for those surgeries – even when it was available – claiming that Black people did not feel pain like whites, despite the need to hold the bondswomen down so they wouldn’t move while they were operated on.
- contributed racial pseudoscience to the medical literature, disparaging and dehumanizing the enslaved as biologically inferior to whites. Their research and writings were flawed and contradictory. They used the bodies of the enslaved to perfect surgeries and they would then use the same techniques on white women. The proof that all women had the same organs and tissues escaped those early physicians. They would attribute poor healing in Black women to hypersexuality – not on being forced to work after surgery and poor nutrition or being raped by their oppressors. White physicians made up diseases which were unique to Black people.
For example: Drapetomania was a conjectural mental illness that, in 1851, American physician Samuel A. Cartwright hypothesized as the cause of enslaved Africans fleeing captivity.
Physicians did not ‘care’ for enslaved people except insofar as they were able to develop surgical techniques and tools or increase the profit off those in bondage.
Contrast that role with that of the Granny Midwife who assisted birthing mothers and cared for the sick and injured and passed down traditional skills and knowledge. This is a rich history which should be further elaborated.
In the late 1800’s to 1960’s doctors organized professional organizations, continued to use Black people to advance their research, and built hospitals. In so doing they:
- convinced women that midwives were dirty, unskilled, and births were far safer in the hospital.
- instituted public policies to prevent midwives from practicing.
- under Jim Crow laws discriminated against descendants of the enslaved by not accepting them as patients in their hospitals
- segregated Black people into separate (and unequal) wards in the North, if they did admit them to the hospital.
- excluded Black physicians from professional organizations and practicing in white serving hospitals.
- perpetuated stereotypes about African Americans in medical research and education.
- Conducted Syphilis Experiment in the Tuskegee Alabama area
- Forced or coerced sterilization on women of color (recent reports of immigrant ICE detainees having unwanted gyn surgeries)
- Used Henrietta Lacks biopsy tissue for scientific advancement without her consent.
From the 1960’s to Present, despite the Civil Rights era and end of Jim Crow laws, structural and institutional racism, and personal bias and stereotypes continue to affect the health of African Americans.
- The determined agenda of white supremacists to preserve white domination generated a concerted backlash to civil rights era laws which impacted social determinants of health. From restricting Medicare to people over 65 to undermining affirmative action (why the % of physicians who are Black is still 5%) to non-expansion of Medicaid in southern states with the Affordable Care Act – just 3 examples of white backlash from the 1960’s to 2000’s affecting health of Black people.
- 1/3 of Black Americans report discrimination in healthcare settings
- 27% of Black mothers report disrespect or abuse while in the hospital to give birth
- 3 to 12 times as many Black mothers die of pregnancy related complications as whites (depending on city/region) in the US
- Black mothers with college degree are 5 times more likely to die than their white counterparts
- California medical professionals implemented improved obstetrical practices between 2005 and 2013 and cut Maternal Mortality in half in that state, but Black women still died at 3x the rate of whites. They are now focusing on racism as a root cause and mandating anti bias training for medical providers.
- 50% of physicians in training believe stereotypes about Black people’s bodies, which affects 40% of treatment decisions
- white doctors spend less time with their patients of color and communicate poorly
- Stress of racism and discrimination have been shown to contribute to many medical conditions including premature births, hypertension and heart disease.
- The theory of ‘Weathering’ or premature aging of Black women’s bodies due to racism has gained more traction in recent years with biological studies supporting physical damage to telomeres, hormonal alterations, and inflammation in the uterus. *Think about Erica Garner who became an activist after her father was choked to death by police in Staten Island. A few years later during her pregnancy she was found to have an enlarged heart. She died of heart problems exacerbated by asthma 4 months postpartum.
- Medical providers often blame patients for bad outcomes saying they were poor historians or noncompliant.
- Despite public health research going back decades and the landmark report ‘Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare’ from the Institute of Medicine in 2003, doctors are mostly in denial that Black lives are not valued when accessing healthcare. The many stories of women who report symptoms of complications and are not listened to provide a different narrative. Take Serena Williams, for example, who knew she was experiencing a pulmonary embolism the day after giving birth by c-section. She was dismissed when she asked for what she knew was life- saving treatment. Only her white husband was heard.
Future
The Pandemic and the masses of people reacting to the deaths of George Floyd and Breonna Taylor, and racial injustice in general, are currently drawing attention to what Public Health experts, Reproductive Justice Activists, and others have been saying for decades – Racism is killing us.
There are movements, some led by Black Women, addressing racial disparities in multiple areas of medicine. These are gaining momentum because of the recent upheavals:
- Movement is Life Caucus – addressing disparities in joint diseases
- Respectful Maternity Care – decreasing disrespect and abuse of birthing people
- Decolonizing Birth – women taking back their roles as life givers – birth workers, Doulas, Midwives caring for birthing people in their communities.
- Black Mamas Matter Alliance – Black women-led cross-sectoral alliance which centers Black Mamas to advocate, drive research, build power, and shift culture for Black maternal health, rights, and justice.
- Health Care Transformation Task Force which runs the Maternal Health Hub
Topics at Upcoming Decolonizing Birth Conference -RJ & BJ stand for Reproductive Birth Justice:
In addition to activists there are progressive politicians pushing for those sociopolitical policies and legislation which are needed to influence environmental injustice, access to healthcare, universal coverage, criminal injustice, discrimination in housing, living wage, etc.
Some examples:
H.R.6142 – Black Maternal Health Momnibus Act of 2020
Green New Deal
Attorney General of Philadelphia Larry Krasner is an innovative Criminal Justice reformer
NYC Standards of Respectful Care at Birth (from Dept of Health in collaboration with community members)
There are many more legal and policy innovations which can have some impact, but often they are band-aids on the abscess of white supremacy in the US. To achieve wealth and health equity will take decades of concerted effort and political will to effect substantive change. What is needed is the dismantling and restructuring of systems which were designed to neglect or oppress Black people.
Researchers are beginning to look at how whiteness influences design of studies, and the language used. Some are centering marginalized groups. Community led or guided research is more common now. There is the idea of studying medical professionals to figure out how to change their behavior with patients.
What the Black Community can do Now to improve Health and Well-being:
- Increase numbers and use of Black midwives, nurses, doulas, physicians
- Healthcare Advocacy – Amplifying Black voices in medical settings for example the ACTT Curriculum of Black Coalition for Safe Motherhood
- Ubuntu – Caring Community
Neighborhood Gardens
Healthy food collectives and food banks
Drive through Baby Showers
Chocolate Milk Caf© (lactation support groups)
Doula Support
Community Health Workers
Community Based health services
Age Friendly Community Initiatives
Holistic Community support for Birthing people
Support Black Owned Businesses (wealth is key to health)
Western Medicine and the Health of the People of the African Diaspora Read More »